Shopping for a new fertility and family building benefit can feel daunting. You’re going to quickly find yourself looking at a mountain of information, piles of data, and solutions that are hard to tell apart.
Fortunately, you can narrow down your search for a benefit much faster when you understand three key things: provider networks, financial models, and clinical outcomes.
Here’s what we’ll cover:
- Understanding Provider Networks
a. What your employees need in a network
b. Types of provider networks
- Clinical Outcomes (and Why They Matter)
a. Data collection and validation
b. Key fertility metrics to look for
Understanding Provider Networks
What your employees need in their network
In fertility, successful pregnancies are more likely when people can find a convenient provider they’re comfortable with, who fits their needs and preferences, and who they trust. Providing your employees with convenient access to and ample choice of high-quality providers is essential to this success.
Access matters because patients will visit their chosen clinic frequently during treatment. Telemedicine visits are great for consultations and check-ups, but there are many required steps during treatment that must be in person. Convenient provider access is key. (Protip: to truly enable access, you’re going to need a network with hundreds of providers. A few dozen clinics spread across the country with only one or even a few providers in each location just won’t cut it.)
Choice is important because your population is diverse, so their choice of providers should be too. Many people on their fertility journey will consult with more than one clinic in the pursuit of a care provider who fits their specific needs and preferences. Your members are going to want access to the top providers first and foremost – and these providers are going to need to be in-network for both physician and embryology lab services.
Quality is critical to family building success. Fertility is a unique area of healthcare where every clinic in the United States reports its outcomes to the CDC. This removes guesswork and provides a baseline to understand and compare quality across providers. However, this data is just a start – and impossible for benefit leaders to monitor regularly to ensure the quality of care their employees are receiving. Having a benefit solution that conducts ongoing quality control of its network for you can make a big difference in not only ensuring your members receive the best care but improve their clinical outcomes and give you peace of mind. Simply put, you want a large network, but not every provider under the sun – only the best providers.
A fertility benefit is only as strong as its provider network. Your employee population is diverse in many ways – racially, medically, financially, and even geographically. Truly equitable benefits offer convenient access to esteemed providers for everyone in your employee population. The more expansive your provider network, the more agency your employees have in finding a provider of choice. The higher the quality of that network, the greater chances your employees have for success. Working with a fertility provider with a limited or low-quality network only limits your employee’s options and access to care.
Types of provider networks

Now that we know to look for access, choice, and quality in a provider network, let’s break down what these provider networks can look like.
A bit of clarification first. A “benefit” or “solution” is the organization that offers the fertility and family building benefit, such as a traditional health insurance plan or a specialized solution like Progyny.
A “provider” or “network” includes the medical organizations and professionals who provide the actual services and treatments.
Sometimes the benefit and network are one in the same. Sometimes they’re two distinct entities. Other times, they’re something in between.
Now, let’s look at four common types of networks you’ll find in the fertility and family building space.
Curated and actively managed networks
In this model, the benefit solution contracts with and manages the providers in its network. These providers must adhere to rigorous standards of inclusion, go through a credentialing process, use the latest technologies, and employ best practices to be included in the network. This ensures consistent provider quality, allows the benefit to have direct access to outcomes data for accurate reporting, and ensures the safest and most effective practices – such as single embryo transfer – are in place at all of their provider clinics. Since the benefit does not own any clinics, there’s no conflict of interest pushing employee members to choose one clinic over another. Active management provides a level of quality control that isn’t available in other networks. This results in a network that provides members with the greatest levels of access, choice, and quality while managing to the best outcomes.
Clinic-owned with a network layer
This is where the benefit owns clinics within their network and contracts with additional clinics to fill in geographic gaps for their clients. When a benefit owns a clinic, they’re incentivized to drive as many patients to that clinic as possible. This creates an inherent conflict with non-owned clinics who have no incentive to join the network and won’t want to share data with their competitor. This also leaves patients with little choice or access. More importantly, it removes the benefit’s objectivity when it comes to caring for your employee population – outcomes reporting doesn’t have to be standardized and there is no ability to control quality.
Carrier network with Centers of Excellence (COEs)
This is a common model you’ll see offered through large general insurance carriers or vendors who sit on top of a carrier network. Like clinic-owned models, they try to drive patients to a select group of specialist providers known as “centers of excellence.” These COEs are very limited in terms of location and variety, so they offer your employees little access or choice when it comes to finding a provider that’s the perfect fit. Many top providers avoid carrier networks because they generally take a one-size-fits-all approach, they require lengthy pre-authorization and utilization reviews, and they have restrictive policies that make it hard for some groups (i.e.; LGBTQ couples, single parents by choice) to get care. They also tend to use a restrictive dollar max financial model, which we’ll get into in the next section.
Discount network for reimbursement models
Discount services? Sign me up, right? Not quite. Discount or reimbursement networks do one thing – slightly decrease prices for services provided by a select group of providers. Simply, this is a fee-for-service model. The benefit is usually a post-tax reimbursement or a “wallet” of funds to use at select providers. These benefits use a dollar max model that turns fertility into a financial decision instead of a medical one (again, more on that next). They have no quality control abilities when it comes to their provider network. They have no ability to capture outcomes data from providers and therefore no effective reporting back to clients. They may offer an expansive network, but since it’s a reimbursement that can be used anywhere, there is no guarantee of quality.
These are the most common types of network models you’ll see in the marketplace. However, your best bet is to find a curated and actively managed network. This type of network is proven to be the most effective for providing access, choice, and quality while ensuring positive patient outcomes.
Next, we’ll look at how these benefits set pricing for access to their services.
Common Benefit Financial Models

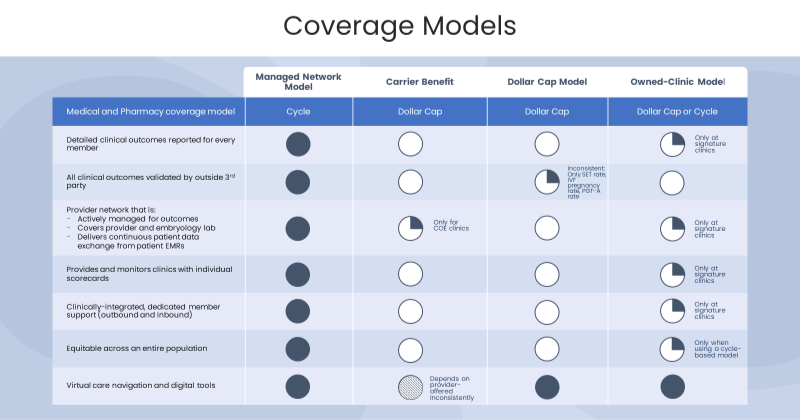
There are two common approaches to covering fertility and family building benefits: fee-for-service (or “dollar max/cap” and “wallet models”) models and value-based care models.
Fee-for-service or Dollar max model
This financial model is simple: it means that every employee has the exact same amount of money to spend at the start of their parenthood journey.
Sounds perfectly equitable right? Think again. If all employees receive $20,000 toward fertility and family building support, a few different things can happen:
- The same procedures may have different costs associated with them depending on where each employee is located. This is especially true for those living in higher-cost metropolitan cities such as New York City or Los Angeles.
- Some employee populations need more care. Same-sex couples and single parents by choice often require additional reproductive intervention that comes with a higher price tag, at no fault of their own. Certain ethnicities are more likely to carry life-threatening conditions that require additional genetic testing (PGT) to help an embryologist select the best embryo to transfer for a healthy pregnancy and healthy baby. These populations hit the dollar max much faster.
- If an employee hits their maximum after one round of IVF, they are left uncovered and child-less if it is unsuccessful. As a result, employees who have a dollar cap benefit are more likely to make price-based care decisions that put everyone’s health at risk (greater costs to your health plan down the line, too!). They may go into personal debt and feel unsupported, and all this leads to lower morale and productivity.
The short of it? Dollar max models are not equal playing fields.
When paired with one size fits all treatment mandates common in the COE carrier network model, fee-for-service models can drive even deeper disparities in plans as coverage is wasted on meeting treatment guidelines that don’t take into consideration individual patient care needs.
Even with the best intentions, this pricing structure can have a negative impact on your employees and leave them feeling disregarded by your organization.
Value-based care model
A value-based model aligns quality and cost – the benefit is designed to cover an entire episode of care and drive to the optimal outcome. This model puts patient needs at the heart of the journey and eliminates any discrepancies or discrimination in the process. By focusing on the patient, this model enables patients and their care teams to make decisions based on treatment needs rather than on what’s left in their wallet.
If a couple requires genetic testing to have a child, it’s covered as part of their journey. If a single parent by choice needs to purchase donor tissue to have a child, it’s covered as part of their journey. If a same-sex female couple needs reciprocal IVF to have a child, it’s covered as part of their journey. The benefit is aligned throughout to incentivize the best care the first time, with quality providers. Sensing a theme? Value-based care is built on aligning cost and quality, and as a result, delivers equitable care that drives optimal outcomes.
The biggest concern with these models is that you may spend more on care than with a dollar max design. However, data shows that the prioritization of the right care, the first time, leads to better outcomes and overall greater cost savings in high-risk intervention and turnover.
This comes back to access, choice, and quality. If a patient finds a provider they’re comfortable with, who uses the best evidence-based best practices and operates in a responsible manner, and who has a well-documented track record of success, you’re much more likely to see a successful pregnancy and healthy baby.
On the other hand, the patient who must drive two hours to her clinic, who doesn’t have confidence in her provider, and who is making decisions based on the last few thousand dollars in her fertility account is going to struggle. She may defer necessary care. She may be stuck with a sub-par clinic. And because her initial care wasn’t optimized, she may need more rounds of treatment.
In fact, Resolve, the National Infertility Association, conducted a study which confirmed that 97% of employers did not see any increase in medical plan costs when adding infertility treatment coverage. Rather, there is greater risk and costs associated with not providing adequate coverage, as 68% of employees said they would leave their existing employer for better fertility coverage.
One bonus of a value-based care model is that in a fertility benefit like Progyny, this care is accompanied by dedicated patient care advocates. They’re full-service guides, available for members who want to call in with questions. They also proactively reach out to members going through the fertility and family building journey to provide support. Combined with digital tools and educational materials, this care model puts the member’s experience, comfort, and outcomes first.
Clinical Outcomes (and Why They Matter)

Data collection and validation
At a very high level, fewer treatments and less medications is the best-case scenario for everyone involved. This will keep costs low and deliver successful babies at a higher rate.
This is what every fertility and family building program strives toward. Luckily, the data is there to tell you if the program is succeeding – so long as you know what to look for.
The first key component is data collection, or how the vendor manages and monitors its program’s success. You’ll want to look for two things:
- Continuous Data Exchange and timely reporting on outcomes for all members allows you (as the employer) to stay abreast of the most accurate outcomes from each clinic, without having to wait for claims data. Having this access allows you to be agile with your benefit dollars rather than responsive.
- External Validation is key. Just like in any industry, you will see claims from organizations that they provide the “best” outcomes. External validation is a tried-and-true way to confirm this. This is the process whereby an external, third-party organization scientifically reviews all outcomes data and validates the organization’s claims.
A best-in-class fertility benefits solution will also collect treatment outcomes data for every patient directly from providers – no samples, no cherry-picking, no projections – simply the ability to report back to employers on their specific populations.
Key fertility metrics to look for
Once you have confirmed your vendor utilizes continuous data exchange and has undergone external validation, the key metrics to understand are as follows:
Single-embryo transfer rate
Elective single-embryo transfer (eSET) is a procedure in which one embryo, selected from a larger number of available embryos, is placed in the uterus or fallopian tube. This is important because it helps women avoid several risks to their own health that are associated with carrying multiples (twins or triplets). There is consensus among experts that the desired outcome of Assisted Reproductive Technology (ART) is a healthy single, or singleton, infant.*
IVF multiples rate
The human womb is made to carry one child to term. Add more and risks for a preterm birth or other pregnancy complications increase. IVF multiple births risks include:
- Almost 60% of twins and 90% of triplets are delivered preterm
- Life-threatening maternal complications are two times higher among twin pregnancies and maternal death rates are almost four times higher with twins
- Multiple births increase the risk of premature birth and low birth weight
Preterm births are especially dangerous. They can lead to infant mortality in serious cases or long-term mental and physical disabilities. Beyond initial neonatal care costs, a pre-term infant may also require continued care for learning difficulties, chronic lung conditions, or immune system problems, among others.**
Miscarriage rate
Unfortunately, miscarriages can happen in the process of fertility treatment. There are lots of reasons for a miscarriage, but there are best practices and procedures that can mitigate the risk of miscarriages during fertility treatment. When examining a benefit, a lower miscarriage rate is typically an indication that the benefit’s providers are taking the necessary precautions and steps to ensure healthier pregnancies.
Understanding these statistics and verifying the quality of an organization’s data for reporting them will ensure your chosen benefit is offering that crucial component of what your employees need: quality.
Bringing it all together

So, let’s recap!
When you’re looking to start or update your fertility and family building benefit, you’ll want to focus on three key areas: provider networks, financial models, and clinical outcomes.
Once you understand those components of each potential benefit, your next step is to evaluate those components against what your employees need in a benefit: access, choice, and quality. In doing so, you’ll have the greatest chance of providing an equitable benefit that sets ALL your employees up for family building success.
For more information about Progyny’s specific coverage and to see if it’s the right fit for your organization, book a demo.
More Resources: Fertility Outcomes Resource Center | Progyny
