Updated by the Progyny Clinical Team — December 2025.
In vitro fertilization (IVF) was originally developed in the early 1970s to help people who had blocked or damaged fallopian tubes. Since then, advances in IVF and other assisted reproductive technologies have led to the birth of millions of babies.
Sometimes IVF alone is not enough, especially when male infertility or a history of poor fertilization in an IVF cycle is present. Intracytoplasmic sperm injection (ICSI) is a laboratory technique developed to help improve fertilization in these situations.
How ICSI works
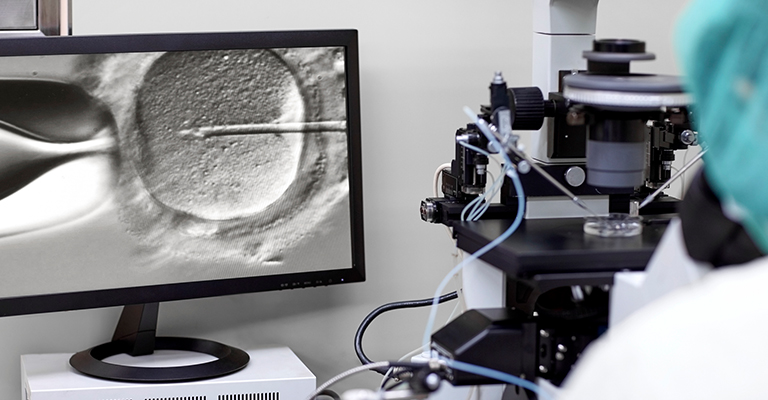
ICSI involves injecting a single sperm directly into an egg outside the body.
Most of the time, sperm comes from ejaculated semen. The lab prepares the ICSI sample by spinning it in a centrifuge to separate live sperm from debris and nonmoving sperm.
If no sperm is found in the ejaculate because of an obstruction, a lack of sperm production, or an ejaculation issue, sperm can sometimes be retrieved surgically from the testes or epididymis. ICSI allows these sperm to be used for fertilization.
After your egg retrieval during an IVF cycle:
- An embryologist stabilizes a mature egg.
- Using a thin micropipette, they guide a single sperm into the egg.
- The sperm is injected into the cytoplasm of the egg.
- The egg is then cultured in the lab and checked the next day for signs of fertilization.
Who may use ICSI
ICSI is most commonly used to address male infertility when fertilization rates may be lower. This includes:
- Low sperm concentration (count)
- Low sperm motility (movement)
- Poor sperm morphology (shape)
Other reasons you may use ICSI include:
- A failed IVF cycle
- Preimplantation genetic testing
- Using previously frozen eggs
- Semen results are borderline or difficult to interpret
- You are an HIV-discordant couple (when only one partner has HIV)
ICSI success rates
The fertilization rate can reach up to 80% when using ICSI. While it does not guarantee fertilization, complete fertilization failure is rare. As with IVF, egg quality and age are the main factors that influence success.
Is ICSI safe?
The outcomes of ICSI are similar to IVF without ICSI, and the same general risks apply.
Some concerns discussed in research include:
- A small increase in the risk of hypospadias, a condition where the opening of the penis is not at the tip.
- Possible links to imprinting disorders, such as Angelman syndrome, though current evidence is limited.
- A slightly higher chance of one embryo splitting into two, especially when transferring a blastocyst.
According to the American Society for Reproductive Medicine, certain rare conditions present at birth — including imprinting disorders, hypospadias, and sex chromosome differences — have been associated with ICSI. These conditions occur in far fewer than 1% of children conceived with ICSI, and the overall increase in risk is small.
Some people with very low sperm counts have underlying genetic conditions that can be passed to children. If this applies to you or your partner, your doctor may recommend genetic screening before treatment.
If you have questions, Progyny is here for you. Please contact your Progyny Care Advocate for support.
Disclaimer: The information provided by Progyny is for educational purposes only and is not medical advice. Always consult a qualified healthcare provider for medical guidance.